Best Medication for Bipolar Depression and Anxiety: Symptoms, Treatment, and Support Strategies
Finding the best medication for bipolar depression and anxiety often feels like trying to solve a puzzle while the pieces are moving. If you feel overwhelmed, you aren’t alone. Bipolar...

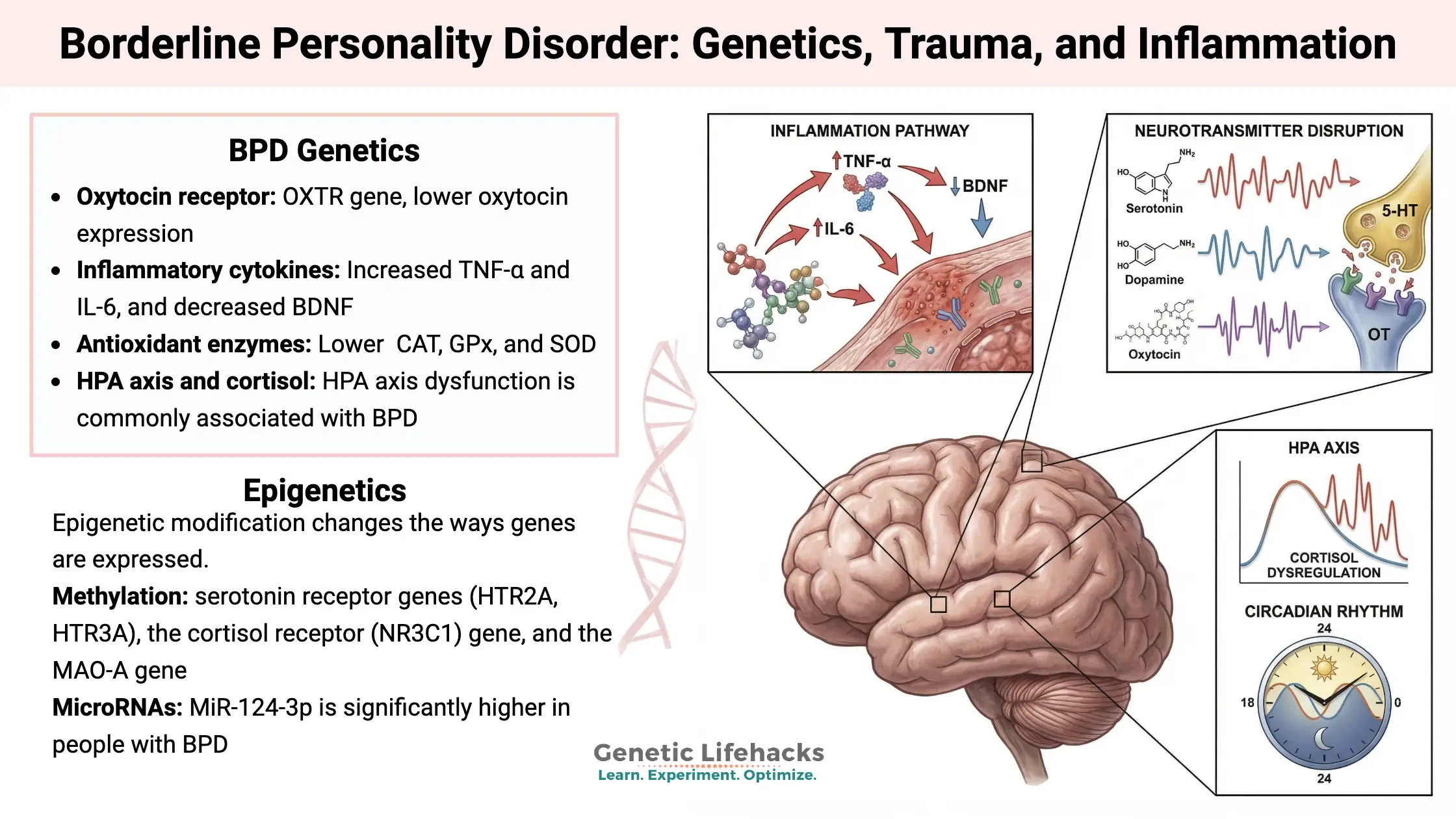
Self-Destructive BPD Symptoms, Petulant BPD & BPD Self-Tests
Navigating the landscape of Borderline Personality Disorder (BPD) often feels like traversing a storm that...
Discouraged Borderline Personality Disorder (Quiet BPD): Symptoms, Causes, Treatment & Real-Life Coping
In my practice, I often meet individuals who feel like “imposters” in the world of...

Recurrent Major Depressive Disorder (ICD-10 & DSM-5): Symptoms, Severity Codes, and Treatment Explained
In my practice, I often observe a specific kind of weariness in patients who are...
Mental Health Conditions
Am I Bipolar?
Explore bipolar disorder basics including symptoms, types (I & II), causes, and more. Get clear, reliable info to better understand this condition and find support.
Bipolar Personality
Does bipolar disorder change your personality? Explore how bipolar affects traits, common misconceptions, and tips for managing identity alongside the condition.
Types of Bipolar
Understand the different types of bipolar disorder – Bipolar I, Bipolar II, cyclothymic, and others – with key differences in symptoms and severity explained.
Bipolar stories
Read inspiring bipolar stories from people living with the condition. Gain hope, insights, and practical tips from real-life journeys of managing bipolar.
Top Reads
Subscribe to Our Newsletter
Get mental health tips, updates, and resources delivered to your inbox.
Featured Stories
Featured Mental Health Topics
Get Support
Read More
Bipolar Disorder Statistics, Facts & Treatment (2026 Guide)
Hey there. Are you looking for the truth behind the numbers? You are not alone in this search. Many people...

Emotional Intelligence: What It Is, Why It Matters, and How to Improve It
In the modern landscape of 2026, where technical skills are increasingly augmented by artificial intelligence, the human element has become...

Anxiety Medication: The Complete Guide to Options, Uses, and Alternatives
Anxiety is a natural human response—a biological alarm system designed to keep us safe from danger. However, for millions of...